Hot Flashes in Menopause
Symptoms, Causes, Risk Factors, and Treatment Options
Hot flashes are the most common symptom associated with menopause. If you are suffering from them, know that you are not alone as 75-80% of women experience hot flashes at some point during menopause.
However, only 20-30% of women ever seek medical attention for their symptoms. Most women develop hot flashes during perimenopause (the years leading up to menopause) but some women will not develop them until they are past the onset of menopause.

Risk Factors for Hot Flashes
Risk factors for hot flashes include obesity, smoking, lack of exercise and ethnicity (incidence is highest for African Americans, followed by Caucasians, and lowest for women of Asian descent particularly Chinese and Japanese).
Duration of Hot Flashes
For most women, hot flashes will last from 6 months – 2 yrs. However, some recent data suggests that up to 10% of women will experience them for more than 10 years after menopause – even into their 70’s!
While menopause is almost always the reason for hot flashes – there can be other rare medical conditions that should not be overlooked.
So, What Is A Hot Flash and What Causes Them?
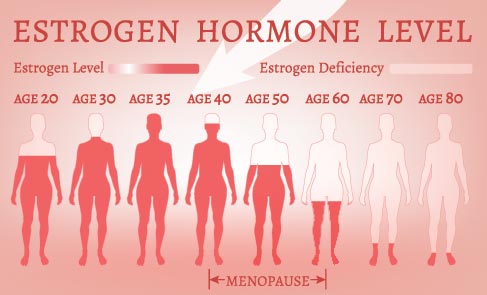
A hot flash is a sudden feeling of heat that starts centrally in the chest area and then spreads to the upper body and face. This process is caused by withdrawal of estrogen which acts on the temperature regulation area of the brain called the hypothalamus. Essentially, the body overreacts to slight changes in core body temperature.
Key Characteristics of Menopausal Hot Flashes
Treatment Options for Hot Flashes
While the symptoms of hot flashes can be troubling, the news is not all bad – there are ways to help you cope with and treat hot flashes.
Behavioral Measures
For mild symptoms, try lowering room temperature, using fans, dressing in layers, losing weight if overweight, and avoiding triggers. For some women, spicy foods and alcohol (particularly red wine) trigger hot flashes.
Hormonal Therapy (HRT)
If deemed medically appropriate – hormones are the most effective way to treat hot flashes.
In addition, hormone replacement can have other benefits such as protecting the bones against osteoporosis and preventing vaginal dryness. HRT will not eliminate all hot flashes but can eliminate most of them and the remainder are typically much more tolerable.
Key Facts about Hormonal Therapy
Several years ago, an oral HRT option with estrogen and Bazodoxifene became available.
Bazodoxifene is an estrogen agonist/antagonist which means that it has estrogen-like effects in some areas of the body and anti-estrogen effects in others. So Bazodoxifene protects the uterus and may be a good option for patients who do not tolerate progesterone. HRT is not without risk, however. There is a small risk of developing a blood clot or DVT when taking estrogen.
Also, when taking estrogen and progesterone together, there can be a slight increase in risk for breast cancer if used for more than 5 years. There are many options available and together with your women’s healthcare provider, you can decide which option is best for you.
“Bio-Identical” Hormones
Quick comment on “bio-identical” hormones.
Initially, this term was a marketing ploy. It refers to using hormones that have the same structure as hormones that are produced by the body. These are typically compounded by specialty pharmacies. However, patients need to be aware that these pharmacies are not regulated so there is no evidence to support that these regimens are any safer than conventional hormone replacement or even effective. They are not recommended as first line therapy by the ACOG.
Non-Hormonal Treatment Options for Hot Flashes
Some women may prefer to not take hormones or may have medical issues that make HRT a contraindication.
Antidepressants
Paroxetine is the only FDA approved option, but providers have seen success with others including venlafaxine, citalopram and escitalopram. When used to treat hot flashes, the relief can start within a few days as opposed to the weeks that the medications can take to treat depression.
Gabapentin
This is a drug that is typically used to treat nerve pain but has shown promise in treating hot flashes. In particular, this seems to work well for night sweats/sleep disturbance as it has a bit of a sedating effect.
Clonidine
This is rarely used any longer due to side effects such as dry mouth, dizziness, and constipation. When it is used, it is typically given as a patch.
Herbal Supplements
Finally, a bit of information about “herbal” supplements.
You may read that black cohosh, soy and Chinese herbal remedies may be useful. Most studies have shown that these options are no more effective than placebo. In addition, these supplements are not regulated by the FDA so they are not monitored for purity or the actual level of active ingredients. These supplements can also interact with other medications, some of them may even be toxic to the liver. If you opt to take any “herbal” supplements, please notify your health care provider.
Get Help with Your Hot Flashes!
In closing, if you are suffering from hot flashes, know that treatment options are available. Please make an appointment to see your Midwest Center for Women’s Healthcare ob/gyn provider. We consider it an honor to provide care for all of our patients.
About the Author
Beth A. Sum, MD, FACOG
Beth Sum, M.D., F.A.C.O.G. is a Board-Certified OB-GYN and a Fellow of the American College of Obstetricians and Gynecologists. She earned her medical degree from Indiana University School of Medicine in Indianapolis and completed her residency at Advocate Lutheran General Hospital in Park Ridge. Dr. Sum is a member of the teaching faculty for the Department of Obstetrics and Gynecology at Advocate Lutheran General Hospital.
Dr. Sum is a devoted Cubs season ticket holder. She and her husband live in Chicago with their son. She loves watching her son’s baseball games and is a devoted hockey Mom. Dr. Sum is accepting new patients by calling 847-318-9359 or requesting an appointment here.